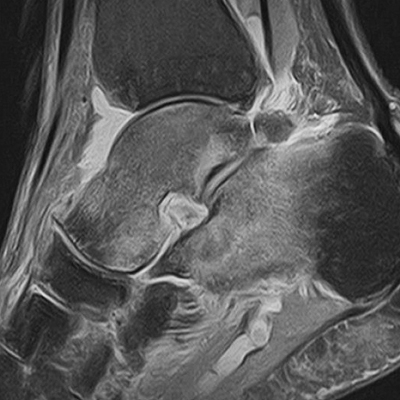
Bone Marrow Edema Following Ankle Ligament Injuries: an MRI Imaging Evaluation
Main Article Content
Abstract
Materials and Methods: We reviewed 50 MRI performed during 2015-2018 for patients who reported ankle pain and signs of instability. Two different radiologists evaluated the series. Bone marrow edema location and specific ligament lesions were contrasted to find possible associations. Chi-Square was used to analyzethe differences.
Results: The anterior talofibular ligament was the most commonly injured ligament (84%). CFL injury occurred in 27 cases (54%). There were no differences between the presence of bone marrow edema and the ligament injured after an ankle sprain (p>0,05). Overall, the most common location of bone marrow edema was the head and neck of the talus (64%). There was no statistical relationship between bone marrow edema location and the injured ligament (p>0,05).
Conclusion: Bone marrow edema is a frequent finding after a ligament injury following ankle sprains. However, this finding is not directly related to a specific location of the injured ligament. The location of bone marrow edema is not related to specific ligament injuries. MRI findings of bone marrow edema must not change the management of patients with acute ankle sprains.
Level of Evidence: II
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
ankle pathologic features with asymptomatic ankles. J Foot Ankle Surg 2011;50:413-5. https://doi.org/10.1053/j.
jfas.2011.03.011
2. Van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical
course of acute ankle sprains? A systematic literature review. Am J Med 2008;121:324-31. https://doi.org/10.1016/j.amjmed.2007.11.018
3. Frey C, Bell J, Teresi L, Kerr R, Feder K. A comparison of MRI and clinical examination of acute lateral ankle
sprains. Foot Ankle Int 1996;17:533-7. https://doi.org/10.1177/107110079601700904
4. Park H-J, Cha S-D, Kim SS, Rho M-H, Kwag H-J, Park N-H, Lee S-Y. Accuracy of MRI findings in chronic lateral
ankle ligament injury: comparison with surgical findings. Clin Radiol 2012;67:313-8. https://doi.org/10.1016/j.
crad.2011.08.025
5. Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am
1976;58:356-7. PMID: 1262367
6. van Putte-Katier N, van Ochten JM, van Middelkoop M, Bierma-Zeinstra SM, Oei EH. Magnetic resonance imaging abnormalities after lateral ankle trauma in injured and contralateral ankles. Eur J Radiol 2015;84:2586-92. https://doi.org/10.1016/j.ejrad.2015.09.028
7. Lee JK, Yao L. Occult intraosseous fracture: magnetic resonance appearance versus age of injury. Am J Sports Med 1989;17:620-3. https://doi.org/10.1177/036354658901700505
8. Deutsch AL, Coel MN, Mink JH. Imaging of stress injuries to bone. Radiography, scintigraphy, and MR imaging.
Clin Sports Med 1997;16:275-90. https://doi.org/10.1016/S0278-5919(05)70022-3
9. Labovitz JM, Schweitzer ME. Occult osseous injuries after ankle sprains: incidence, location, pattern, and age. Foot Ankle Int 1998;19:661-7. https://doi.org/10.1177/107110079801901003
10. Saxena A, Eakin C. Articular talar injuries in athletes: results of microfracture and autogenous bone graft. Am J Sports Med 2007;35:1680-7. https://doi.org/10.1177/0363546507303561
11. Harmon KG. The ankle examination. Prim Care 2004;31:1025-37. https://doi.org/10.1016/j.pop.2004.07.008
12. Konradsen L, Voigt M, Højsgaard C. Ankle inversion injuries. The role of the dynamic defense mechanism. Am J Sports Med 1997;25:54-8. https://doi.org/10.1177/036354659702500110
13. Longo UG, Loppini M, Berton A, Marinozzi A, Maffulli N, Denaro V. The FIFA 11+ program is effective in
preventing injuries in elite male basketball players: a cluster randomized controlled trial. Am J Sports Med
2012;40(5):996-1005. https://doi.org/10.1177/0363546512438761
14. Nishimura G, Yamato M, Togawa M. Trabecular trauma of the talus and medial malleolus concurrent with lateral collateral ligamentous injuries of the ankle: evaluation with MR imaging. Skeletal Radiol 1996;25:49-54. https://doi.org/10.1007/s002560050031