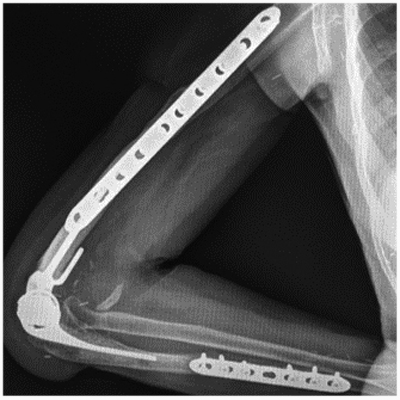
Total elbow arthroplasty after an infection process. Two stage surgery
Main Article Content
Abstract
Material and methods: the inclusion criteria, the diagnosis of infection and the 2 surgical stages are described.
Results: 10 patients were included (7 men and 3 women), average age: 62 years old. Initial causes: degenerative in 2 cases and traumatic in 8. 4 alloprostheses and 2 latissimus dorsi flaps were performed.Follow-up was 5 years. Flexo-extension was 117°/29° in preoperative and 130°/29° in postoperative; pain according to EVA: 6.5 and 2.5; MEPS: 40 and 80; DASH 56 and 30 respectively. The extension force was M5 (4 cases), M4 (2), M3 (1), M1 (2) and M0 (1). One patient presented a necrosis of the flap that evolved with infection. In 9 of the 10 cases the patients were free of infection at the end of the follow-up. Two groups of patients were identified: Group A (bone defects less than 4 cm) and B (more than 4 cm). Group A patients had fewer previous surgeries and better functional outcomes.
Conclusion: the treatment of an infectious elbow process through the placement of antibiotic cement spacer, allows a control of the infection in a high percentage of cases. Secondary prosthetic reconstruction is demanding and associated with complications. It is to be expected that the greater the bone defect and the greater the number of previous procedures, result in the worse the functional results.
Level of Evidence: IV
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
Survival analysis of 113 consecutive cases. J Bone Joint Surg Br 1994;76(4):636-40. PMID: 8027155
2. Wolfe SW, Figgie MP, Inglis AE, Bohn WW, Ranawat CS. Management of infection about total elbow prostheses. J Bone Joint Surg Am 1990;72(2):198-212. PMID: 2303506
3. Yamaguchi K, Adams RA, Morrey BF. Semiconstrained total elbow arthroplasty in the context of treated previous infection. J Shoulder Elbow Surg 1999;8(5):461-5. https://doi.org/10.1016/s1058-2746(99)90077-0
4. Rudge WBJ, Eseonu K, Brown M, Warren S, Majed A, Bayley IL, et al. The management of infected elbow
arthroplasty by two-stage revision. J Shoulder Elbow Surg 2018;27(5):879-86.
https://doi.org/10.1016/j.jse.2017.12.033
5. Kunutsor SK, Beswick AD, Whitehouse MR, Blom AW. One- and two-stage surgical revision of infected elbow
prostheses following total joint replacement: a systematic review. BMC Musculoskelet Disord 2019;20(1):467.
https://doi.org/10.1186/s12891-019-2848-x
6. Kwak JM, Kholinne E, Sun Y, Kim MS, Koh KH, Jeon IH. Clinical results of revision total elbow arthroplasty:
comparison of infected and non-infected total elbow arthroplasty. Int Orthop 2019;43(6):1421-7.
https://doi.org/10.1007/s00264-018-4267-2
7. Watts AC, Duckworth AD, Trail IA, Rees J, Thomas M, Rangan A. Scoping review: Diagnosis and management of
periprosthetic joint infection in elbow arthroplasty. Shoulder Elbow 2019;11(4):282-91.
https://doi.org/10.1177/1758573218789341
8. Gallucci G, Gonzalez D, Boretto J, Alfie V, Donndorff A, De Carli P. Artroplastía total del codo posterior a una
artritis séptica. Rev Asoc Argent Ortop Traumatol 2010;75(3):287-92. LILACS ID: lil-568777
9. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH
(disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J
Ind Med 1996;29:602-8. https://doi.org/10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L
10. Morrey B. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone J Surg Am 1990;72:601-18. PMID: 2324148
11. Florence JM, Pandya S, King WM, J D Robison, J Baty, J P Miller, et al. Intrarater reliability of manual muscle test
(Medical Research Council scale) grades in Duchenne’s muscular dystrophy. Phys Ther 1992;72(2):115-126.
https://doi.org/10.1093/ptj/72.2.115
12. Morrey BF, Bryan RS, Dobyns JH, Linscheld RL. Total elbow arthroplasty. A five-year experience at the Mayo
Clinic. J Bone Joint Surg Am 1981;63:1050-63. PMID: 7276042
13. Hastings H 2nd, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and
forearm. Hand Clin 1994;10(3):417-37. PMID: 7962148
14. Kusnezov N, Dunn JC, Stewart J, Mitchell JS, Pirela-Cruz M. Acute limb shortening for major near and complete
upper extremity amputations with associated neurovascular injury: a review of the literature. Orthop Surg
2015;7(4):306-16. https://doi.org/10.1111/os.12213
15. Mirra JM, Maeder RA, Amstutz HC. The pathology of failed total joint arthroplasty. Clin Orthop 1982;170:175-83. PMID: 7127944
16. Moro JK, King GJ. Total elbow arthroplasty in the treatment of posttraumatic conditions of the elbow. Clin Orthop Relat Res 2000;(370):102-14. https://doi.org/10.1097/00003086-200001000-00010
17. Lovy AJ, Keswani A, Dowdell J, Koehler S, Kim J, Hausman MR. Outcomes, complications, utilization trends, and
risk factors for primary and revision total elbow replacement. J Shoulder Elbow Surg 2016;25(6):1020-1026.
https://doi.org/10.1016/j.jse.2015.12.012
18. Prkic A, Welsink C, The B, van den Bekerom MPJ, Eygendaal D. Why does total elbow arthroplasty fail today? A
systematic review of recent literature. Arch Orthop Trauma Surg 2017;137(6):761-9. https://doi.org/10.1007/s00402-017-2687-x
19. Zmistowski B, Pourjafari A, Padegimas EM, Sheth M, Cox RM, Ramsey ML, et al. Treatment of periprosthetic
joint infection of the elbow: 15-year experience at a single institution. J Shoulder Elbow Surg 2018;27(9):1636-41.
https://doi.org/10.1016/j.jse.2018.05.035
20. Peach CA, Nicoletti S, Lawrence TM, Stanley D. Two-stage revision for the treatment of the infected total elbow arthroplasty. Bone Joint J Br 2013;95(12):1681-6. https://doi.org/10.1302/0301-620X.95B12.31336
21. Gutman MJ, Stone MA, Namdari S, Abboud JA. Treatment of elbow periprosthetic joint infection: a systematic
review of clinical outcomes. J Shoulder Elbow Surg 2020;29(2):411-9. https://doi.org/10.1016/j.jse.2019.10.002
22. Rhee YG, Cho NS, Park JG, Song JH. Resection arthroplasty for periprosthetic infection after total elbow
arthroplasty. J Shoulder Elbow Surg 2016;25(1):105-11. https://doi.org/10.1016/j.jse.2015.08.045
23. Cheung EV, Adams RA, Morrey BF. Reimplantation of a total elbow prosthesis following resection arthroplasty for infection. J Bone Joint Surg Am 2008;90(3):589-94. https://doi.org/10.2106/JBJS.F.00829
24. Allende C, Mangupli M, Bagliardelli J, Díaz P, Allende BT. Infected nonunions of long bones of the upper
extremity: staged reconstruction using polimethylmethacrylate and bone graft impregnated with antibiotics. Chir Organi Mov 2009;93(3):137-42. https://doi.org/10.1007/s12306-009-0046-y
25. Somerson JS, Morrey ME, Sanchez-Sotelo J, Morrey BF. Diagnosis and management of periprosthetic elbow
infection. J Bone Joint Surg Am 2015;97(23):1962-71. https://doi.org/10.2106/JBJS.O.00170
26. Pelissier A, Masquelet R, Bareille S. Induced membranes secrete growth factors including vascular and
osteoinductive factors and could stimulate bone regeneration. J Orthop Res 2004;22:73-9.
https://doi.org/10.1016/S0736-0266(03)00165-7
27. Duquin TR, Jacobson JA, Schleck CD, Larson DR, Sanchez-Sotelo J, Morrey BF. Triceps insufficiency after the
treatment of deep infection following total elbow replacement. Bone Joint J Br 2014;96(1):82-7.
https://doi.org/10.1302/0301-620X.96B1.31127