Supracondylar Subtraction Wedge Osteotomy for the Treatment of Adult Cubitus Valgus
Main Article Content
Abstract
Materials and methods: 5 patients were included. The surgical technique consisted of a posterior paratricipital approach, with resection of a subtractive wedge and the anterior transposition of the ulnar nerve. The average follow-up was 17 months.
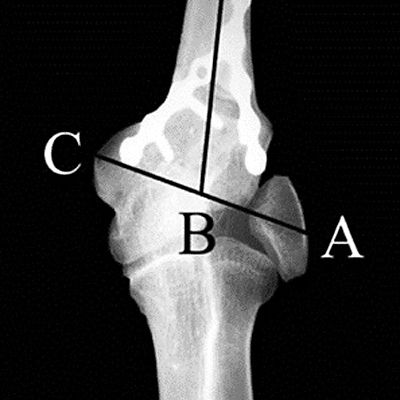
Results: 4 patients were men and 1 was a woman with an average age of 27 years. The preoperative range of motion was 138°-7° and the postoperative range of motion was 138-6°. Pain according to VAS was 4 and 1, MEPS was 71 and 97, and DASH 6 was 26 and 8, respectively. The preoperative radiological evaluation showed an average valgus of 30º with a contralateral valgus of 11°. The final valgus obtained was 13º. The final correction was, on average, 2° less than the contralateral side. All osteotomies healed and the medial prominence was on average 32% more than before surgery. According to the Oppenheim scale, the results were excellent in 4 patients and good in 1. Personal satisfaction was, on average, 8.6.
Conclusions: Supracondylar subtractive wedge osteotomy is a good option for the treatment of adult cubitus valgus, with a recovery of angular values similar to the contralateral side and a high satisfaction rate. As it is a simpler technique, compared to the multiplanar osteotomies, it is our treatment of choice for adult cubitus valgus.
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
2. Storm SW, Williams DP, Khoury J, Lubahn JD. Elbow deformities after fracture. Hand Clin 2006;22(1):121-9.
https://doi.org/10.1016/j.hcl.2005.12.005
3. Bub FR, Schulz AP, Lill H, Voigt C. Supracondylar osteotomies of posttraumatic distal humeral deformities in
young adults-technique and results. Open Orthop J 2011;5:389-94. ttps://doi.org/10.2174/1874325001105010389
4. Labelle H, Bunnell WP, Duhaime M, Poitras B. Cubitus varus deformity following supracondylar fractures of the
humerus in children. J Pediatr Orthop 1982;2(5):539-46. https://doi.org/10.1097/01241398-198212000-00014
5. Wilkins KE. Fractures and dislocations of the elbow region. En: Rockwood CA, Wilkins KE, King RE (eds.).
Fractures in children, 4th ed. Philadelphia: Lippincott-Raven; 1996:600-887.
6. Amspacher JC, Messenbaugh JF Jr. Supracondylar osteotomy of the humerus for correction of rotational and
angular deformities of the elbow. South Med J 1964; 57:846-50. https://doi.org/10.1097/00007611-196407000-00022
7. Kang HJ, Koh IH, Jeong YC, Yoon TH, Choi YR. Efficacy of combined osteotomy and ulnar nerve transposition for
cubitus valgus with ulnar nerve palsy in adults. Clin Orthop Relat Res 2013;471(10):3244-50.
https:doi.org./10.1007/s11999-013-3057-9
8. Kim HT, Lee JS, Yoo CI. Management of cubitus varus and valgus. J Bone Joint Surg Am 2005;87:771-80.
https://doi.org/10.2106/JBJS.D.01870
9. Wong HK, Lee EH, Balasubramaniam P. The lateral condylar prominence. A complication of supracondylar
osteotomy for cubitus varus. J Bone Joint Surg Br 1990;72:859-61. PMID: 2211772
10. Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma 1964;4:592-607.
https://doi.org/10.1097/00005373-196409000-00004
11. Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH
(Disabilities of the Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J
Ind Med 1996;29:602-8. https://doi.org/10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L
12. Morrey BF, An KN, Chao EYS. Functional evaluation of the elbow. En: Morrey BF (ed.). The elbow and its
disorders. 2nd ed. Philadelphia, PA: WB Saunders Co.; 1993:95.
13. Oppenheim WL, Clader TJ, Smith C, Bayer M. Supracondylar humeral osteotomy for traumatic childhood cubitus varus deformity. Clin Orthop Relat Res 1984;188:34-9. PMID: 6467726
14. Abed Y, Nour K, Kandil YR, El-Negery A. Triple management of cubitus valgus deformity complicating neglected nonunion of fractures of lateral humeral condyle in children: a case series. Int Orthop 2018;42(2):375-84. https://doi.org/10.1007/s00264-017-3709-6
15. Tachdjian MR. Osteotomy of distal humerus for correction of cubitus varus. En: Smith AB (ed.). Pediatric
orthopedics. Philadelphia: WB Saunders; 1972:1588-91.
16. Roye DP Jr, Bini SA, Infosino A. Late surgical treatment of lateral condylar fractures in children. J Pediatr Orthop 1991;11:195-9. https://doi.org/10.1097/01241398-199103000-00011
17. Fontanetta P, Mackenzie DA, Rosman M. Missed, maluniting, and malunited fractures of the lateral humeral
condyle in children. J Trauma 1978;18:329-35. https://doi.org/10.1097/00005373-197805000-00006