Functional and radiologic outcomes of reverse shoulder arthroplasty and greater tuberosity reattachment in proximal humerus fractures
Main Article Content
Abstract
Objective: To report functional and radiologic outcomes of reverse shoulder arthroplasty (RSA) in patients with complex proximal humeral fractures. A second objective was to assess the relation between the greater tuberosity healing and the range of motion (ROM) and the American Shoulder and Elbow Surgeons (ASES) score.
Materials and Methods: Sixteen patients treated between 2013 and 2017, older than 65 years old, operated before 4 weeks after the trauma, and with a minimum of 2-year follow-up were included. ASES scores and active ROMs were recorded. Greater tuberosity and the prosthesis position and healing were radiologically evaluated, and the complications and treatment were recorded.
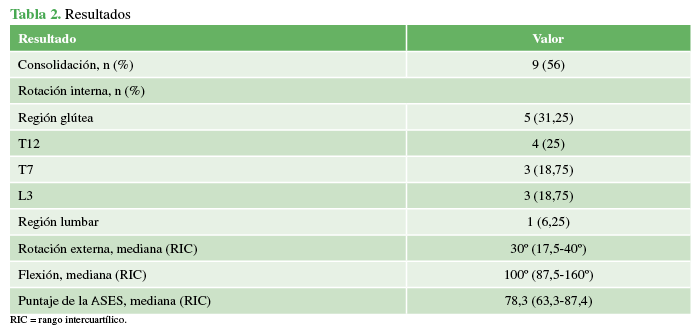
Results: The median age was of 74.5 years (IQR 66-78.5), 11 patients were females (69%). According to Neer classification, 11 cases were four-part fractures and 5 were four-part fracture-dislocations. The average time between trauma and surgery was 9.4 days, and the average follow-up was of 29.5 months. The greater tuberosity was healed in 9 cases (56%). Internal rotation: 5 patients (31.25%) were able to reach up with their thumbs to gluteal level, 4 (25%) to T12, 3 (18.75%) to T7, and 4 (25%) to L3. The medians for external rotation and forward flexion were 30° (IQR 17.5°-40°) and 100° (IQR 87.5°-160°). The average ASES score was of 78.3 (IQR 63.3-87.4). There was no significant statistical relation between greater tuberosity healing and forward flexion or ASES score (P=0.24 and P=0.52, respectively).
Conclusion: The use of reverse prostheses for complex fractures with greater tuberosity reattachment could lead to good functional outcomes, low complication rates and reoperations. There was no significant statistical relation between ASES score and greater tuberosity healing or failure to heal.
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
2. Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three-and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 2007;89(4):516-20. https://dx.doi.org/10.1302/0301-620X.89B4.18435
3. Chun YM, Kim DS, Lee DH, Shin SJ. Reverse shoulder arthroplasty for four-part proximal humerus fracture in elderly patients: can a healed tuberosity improve the functional outcomes? J Shoulder Elbow Surg 2017;26(7):1216-21. https://dx.doi.org/10.1016/j.jse.2016.11.03410.1302/0301-620X.89B4.18435
4. Garofalo R, Flanagin B, Castagna A, Lo EY, Krishnan SG. Reverse shoulder arthroplasty for proximal humerus fracture using a dedicated stem: radiological outcomes at a minimum 2 years of follow-up—case series. J Orthop Surg Res 2015;10:129. https://dx.doi.org/10.1186/s13018-015-0261-1
5. Grubhofer F, Wieser K, Meyer DC, Catanzaro S, Beeler S, Riede U, et al. Reverse total shoulder arthroplasty for acute head-splitting, 3- and 4-part fractures of the proximal humerus in the elderly. J Shoulder Elbow Surg 2016;25(10):1690-8. https://dx.doi.org/10.1016/j.jse.2016.02.024
6. Uzer G, Yildiz F, Batar S, Binlaksar R, Elmadag M, Kus G, et al. Does grafting of the tuberosities improve the functional outcomes of proximal humeral fractures treated with reverse shoulder arthroplasty? J Shoulder Elbow Surg 2017;26(1):36-41. http://dx.doi.org/10.1016/j.jse.2016.05.005
7. Boileau P, Krishnan SG, Tinsi L,Walch G, Coste JS, Molé D. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 2002;11(5):401-12. https://doi.org/10.1067/mse.2002.124527
8. Sebastiá-Forcada E, Cebrián-Gómez R, Lizaur-Utrilla A, Gil-Guillén V. Reverse shoulder arthroplasty versus hemiarthroplasty for acute proximal humeral fractures. A blinded, randomized, controlled, prospective study. J Shoulder Elbow Surg 2014;23(10):1419-26. https://dx.doi.org/10.1016/j.jse.2014.06.035
9. Formaini NT, Everding NG, Levy JC, Rosas S. Tuberosity healing after reverse shoulder arthroplasty for acute proximal humerus fractures: the “black and tan” technique. J Shoulder Elbow Surg 2015;24(11):e299-306. https://dx.doi.org/10.1016/j.jse.2015.04.014
10. Levy JC, Badman B. Reverse shoulder prosthesis for acute four-part fracture: tuberosity fixation using a horseshoe graft. J Orthop Trauma 2011;25(5):318-24. https://dx.doi.org/10.1097/BOT.0b013e3181f22088
11. Boileau P, Krishnan SG, Tinsi L, Walch G, Coste JS, Molé D. Tuberosity malposition and migration: reasons for poor outcomes after hemiarthroplasty for displaced fractures of the proximal humerus. J Shoulder Elbow Surg 2002;11(5):401-12. https://dx.doi.org/10.1067/mse.2002.124527
12. Boileau P, Winter M, Cikes A, Han Y, Carles M, Walch G, et al. Can surgeons predict what makes a good hemiarthroplasty for fracture? J Shoulder Elbow Surg 2013;22(11):1495-506. https://dx.doi.org/10.1016/j.jse.2013.04.018
13. Matthewson G, Kooner S, Kwapisz, A, Leiter J, Old J, MacDonald P. The effect of subscapularis repair on dislocation rates in reverse shoulder arthroplasty: a meta-analysis and systematic review. J Shoulder Elbow Surg 2019;28(5):989-97. https://dx.doi.org/10.1016/j.jse.2018.11.069
14. Cazeneuve JF, Cristofari DJ, Charalambous CP, Abiddin Z, Mills SP, Rogers S, et al. The reverse shoulder prosthesis in the treatment of fractures of the proximal humerus in the elderly. J Bone Joint Surg Br 2010;92(4):535-9. https://dx.doi.org/10.1302/0301-620X.92B4.22450
15. Gallinet D, Adam A, Gasse N, Rochet S, Obert L. Improvement in shoulder rotation in complex shoulder fractures treated by reverse shoulder arthroplasty. J Shoulder Elbow Surg 2013;228(1):38-44. https://dx.doi.org/10.1016/j.jse.2012.03.011
16. Klein M, Juschka M, Hinkenjann B, Scherger B, Ostermann PA. Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 2008;22(10):698-704. https://dx.doi.org/10.1097/BOT.0b013e31818afe40
17. Boileau P, Alta TD, Decroocq L, Sirveaux F, Clavert P, Favard L, et al. Reverse shoulder arthroplasty for acute fractures in the elderly: is it worth reattaching the tuberosities? J Shoulder Elbow Surg 2019;28(3):437-44. https://dx.doi.org/10.1016/j.jse.2018.08.025
18. Ohl X, Bonnevialle N, Gallinet, D, Ramdane N, Valenti P, Decroocq J, et al. How the greater tuberosity affects clinical outcomes after reverse shoulder arthroplasty for proximal humeral fractures. J Shoulder Elbow Surg 2018;27(12):2139-44. https://dx.doi.org/10.1016/j.jse.2018.05.030