Bösch vs MICA Techniques in Hallux Valgus Surgery. Medium-Term Prospective Comparative Radiographic Analysis Español
Main Article Content
Abstract
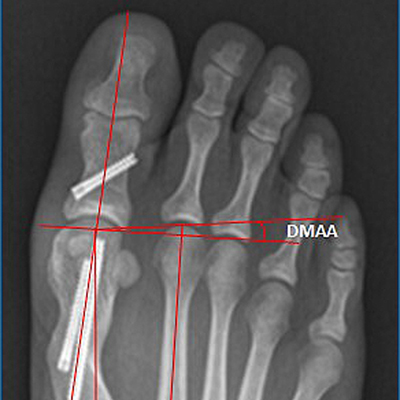
Materials and methods: Prospective comparative analysis of surgically treated patients with hallux valgus by two percutaneous techniques (BOSCH group: 42 feet; MICA group: 36 feet) in homogenous groups. Intermetatarsal, metatarsophalangeal and distal metatarsal articular angle corrections were compared, as well as the correction power of both osteotomies and its stability in the middle term. Postoperative complications were recorded. Minimum follow-up: 6 months.
Results: Average angle correction of MTP, IM y DMAA 6 months after surgery in Bosch group: 20,22°; 7,74°; 8,26°; MICA: 15,8°; 1,6° and 1,98° respectively. BOSCH group had a higher IM correction power. There were no significant statistical differences between both groups in the loss of correction by 6 weeks to 6 months; except for the MTP angle in the MICA group. MICA presented a better correction of the DMAA in time. Postoperatively, MICA had 4 complications, while BOSCH 8.
Conclusions: We obtained good results with both techniques in the treatment of moderate hallux valgus. However, patients undergoing the Bosch technique had greater correction on the intermetatarsal angle in the mid-term follow-up. Although the MTP angle correction decreased between 6 weeksand 6 months in MICA technique, the values remained within normal 20° of valgus MTP.
Level of Evidence: II
Downloads
Metrics
Article Details
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
Elsevier; 2014.
2. Mann RA, Coughlin MJ. Hallux valgus-etiology, anatomy, treatment and surgical considerations. Clin Orthop Relat Res 1981;157:31-41. PMID: 7249460
3. Coughlin MJ, Thompson FM. The high price of high-fashion footwear. Instr Course Lect 1995;44:371-7.
PMID: 7797875
4. Coughlin MJ. Hallux valgus in men: effect of the distal metatarsal articular angle on halux valgus correction. Foot Ankle Int 1997;18:463-70. https://doi.org/10.1177/107110079701800802
5. Amor RT. Pierna, tobillo y pie. Buenos Aires: Cámara Argentina del Libro; 2009.
6. Austin DW, Leventen EO. A new osteotomy for hallux valgus. Clin Orthop Relat Res 1981;157:25. PMID: 7249456
7. Schneider W, Aigner N, Pinggera O, Knahr K. Chevron osteotomy in hallux valgus. Ten-year results of 112 cases. J Bone Joint Surg Br 2004;86(7):1016-20. https://doi.org/10.1302/0301-620X.86B7.15108
8. Maffulli N, Longo UG, Marinozzi A, Denaro V. Hallux valgus: effectiveness and safety of minimally invasive
surgery. A systematic review. Br Med Bull 2011;97:149-67. https://doi.org/10.1093/bmb/ldq027
9. Bösch P, Markowski H, Rannicher V. Technik und erste ergebnisse der subkutanen distalen metatarsale-Iosteotomie. Orthopädische Praxis 1990;26:51-6.
10. Sotelano P, Migues A. Tratamiento percutáneo del hallux valgus. Técnica de Bosch. Rev Asoc Argent Ortop
Traumatol 2007;72(3):233-41. https://www.aaot.org.ar/revista/2007/n3_vol72/art5.pdf
11. Redfern D, Vernois J, Legre BP. Percutaneous surgery of the forefoot. Clin Podiatr Med Surg 2015;32:291-332.
https://doi.org/10.1016/j.cpm.2015.03.007
12. Redfern D, Vernois J. Minimally invasive Chevron Akin (MICA) for correction of hallux valgus. Tech Foot Ankle
Surg 2106;15(1):3-11. https://doi.org/10.1097/BTF.0000000000000102
13. Perera AM, Redfern A, Singh D, Lomax A. Minimally invasive forefoot surgery. J Trauma Orthop 2015;3(1):50-5.
14. Coughlin MJ. Instructional Course Lectures, The American Academy of Orthopaedic Surgeons – Hallux valgus. J Bone Joint Surg Am 1996;78:932-66.
15. Chiang CC, Lin CF, Tzeng YH. Distal linear osteotomy compared to oblique diaphyseal osteotomy in moderate to severe hallux valgus. Foot Ankle Int 2012;33:479-86. https://doi.org/10.3113/FAI.2012.0479
16. Miller JW. Distal first metatarsal displacement osteotomy: its place in the schema of bunion surgery. J Bone Joint Surg Am 1974;56:923-31. http://citeseerx.ist.psu.edu/viewdoc/downloaddoi=10.1.1.1033.3979&rep=rep1&type=pdf
17. Deenik AR, de Visser E, Louwerens JWK, Malefijt MW, Draijer FF, de Bie RA. Hallux valgus
angle as main predictor for correction of hallux valgus. BMC Musculoskelet Disord 2008;9:70. https://doi.org/10.1186/1471-2474-9-70
18. Bosch P, Wanke S, Legenstein R. Hallux valgus correction by the method of Bosch: a new technique with a sevento-ten-year follow-up. Foot Ankle Clin 2000;5(3):485-98. PMID: 11232393
19. Portaluri M. Hallux valgus correction by the method of Bösch: a clinical evaluation. Foot Ankle Clin 2000;5(3):499-511. PMID: 11232394
20. Magnan B, Samaila E, Viola G, Bartolozzi P. Minimally invasive retrocapital osteotomy of the first metatarsal in
hallux valgus deformity. Oper Orthop Traumatol 2008;20(1):89-96. https://doi.org/10.1007/s00064-008-1231-0
21. Giannini S, Faldini C, Vannini F, Bevoni R, Biagini C. Surgical treatment of hallux valgus: a clinical prospective
randomized study comparing linear distal metatarsal osteotomy with scarf osteotomy. Orthop Proceed
2009;91B(Supp I):162.
22. Brogan K. Minimally invasive and open distal Chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int 2016;37(11):1197-1204. https://doi.org/10.1177/1071100716656440
23. Vernois J, Redfern D. Percutaneous surgery for severe hallux valgus. Foot Ankle Clin 2016;21(3):479-93. https://doi.org/10.1016/j.fcl.2016.04.002
24. Iannó B, Familiari F, De Gori M, Galasso O, Ranuccio F, Gasparini G. Midterm results and complications after
minimally invasive distal metatarsal osteotomy for treatment of hallux valgus. Foot Ankle Int 2013;34(7):969-77.
https://doi.org/10.1177/1071100713481453