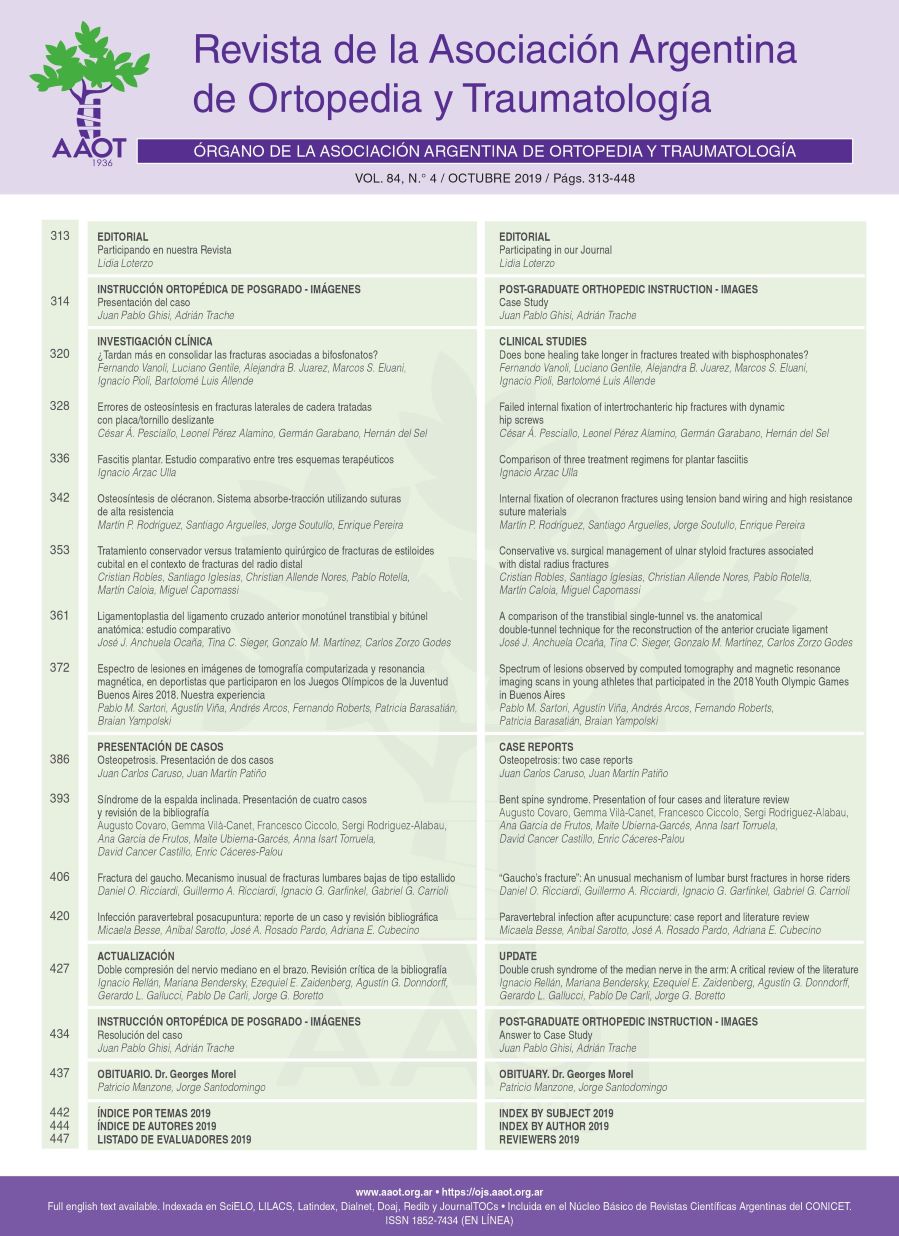
Conservative vs. surgical management of ulnar styloid fractures associated with distal radius fractures
Main Article Content
Abstract
Materials and Methods: This was a multicenter, retrospective and descriptive study including surgical patients treated at four different institutions between 2009 and 2012 for ulnar styloid fractures associated with unstable distal radius fractures. Ulnar styloid fractures were treated conservatively in group I and surgically in group II.
Results: The average follow-up was 56 months. The study included 57 patients divided into two groups (group I [29 cases] and group II [28 cases]). Patients in group II had 2.76 times (95% CI: 1.086; 8.80) more chances of achieving bone union than those in group I. DASH and pain scores, both at rest and during activity, did not show significant differences between the two groups (p = 0.276 and p = 0.877). Group I presented milder ulnar deviation and better strength (p = 0.0194 and p = 0.024).
Conclusions: Although patients who underwent surgery for ulnar styloid fractures had 2.76 more chances of achieving bone union than those who received conservative management, there were no significant differences between both groups in subjective evaluations (DASH and pain scores) or when considering the degree of ulnar styloid involvement. However, the parameters of strength and ulnar deviation were better in the conservative management group.
Downloads
Metrics
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Manuscript acceptance by the Journal implies the simultaneous non-submission to any other journal or publishing house. The RAAOT is under the Licencia Creative Commnos Atribución-NoComercial-Compartir Obras Derivadas Igual 4.0 Internacional (CC-BY-NC.SA 4.0) (http://creativecommons.org/licences/by-nc-sa/4.0/deed.es). Articles can be shared, copied, distributed, modified, altered, transformed into a derivative work, executed and publicly communicated, provided a) the authors and the original publication (Journal, Publisher and URL) are mentioned, b) they are not used for commercial purposes, c) the same terms of the license are maintained.
In the event that the manuscript is approved for its next publication, the authors retain the copyright and will assign to the journal the rights of publication, edition, reproduction, distribution, exhibition and communication at a national and international level in the different databases. data, repositories and portals.
It is hereby stated that the mentioned manuscript has not been published and that it is not being printed in any other national or foreign journal.
The authors hereby accept the necessary modifications, suggested by the reviewers, in order to adapt the manuscript to the style and publication rules of this Journal.
References
2. Sachar K. Ulnar-sided wrist pain: evaluation and treatment of triangular fibrocartilage complex tears, ulnocarpal impaction syndrome and lunotriquetral ligament tears. J Hand Surg Am 2012;37:1489-500. https://doi.org/10.1016/j.jhsa.2012.04.036
3. Ali M, Brogren E, Wagner P, Atroshi I. Association between distal radial fracture malunion and patient reported activity limitations. J Bone Joint Surg Am 2018;100:633-9. https://doi.org/10.2106/JBJS.17.00107
4. Sammer DM, Chung KC. Management of the distal radioulnar joint and ulnar styloid fracture. Hand Clin 2012;28:199-206. https://doi.org/10.1016/j.hcl.2012.03.011
5. Souer JS, Ring D, Matschke S, Audige L, Marent-Huber M, Jupiter JB. Effect of an unrepaired fracture of the ulnar styloid base on outcome after plate-and-screw fixation of a distal radial fracture. J Bone Joint Surg Am 2009;91:830-8. https://doi.org/10.2106/JBJS.H.00345
6. Wijffels MM, Keizer J, Buijze GA, Zenke Y, Krijnen P, Schep NW, et al. Ulnar styloid process nonunion and outcome in patients with a distal radius fracture: a meta-analysis of comparative clinical trials. Injury 2014;45(12):1889-95. https://doi.org/10.1016/j.injury.2014.08.007
7. Buijze GA, Ring D. Clinical impact of united versus non-united fractures of the proximal half of the ulnar styloid following volar plate fixation of the distal radius. J Hand Surg Am 2010;35:223-7. https://doi.org/10.1016/j.jhsa.2009.10.035
8. May MM, Lawton JN, Blazar PE. Ulnar styloid fractures associated with distal radius fractures: incidence and implications for distal radioulnar joint instability. J Hand Surg Am 2002;27:965-71. https://doi.org/10.1053/jhsu.2002.36525
9. Sammer DM, Shah HM, Shauver MJ, Chung KC. The effect of ulnar styloid fractures on patient-rated outcomes after volar locking plating of distal radius fractures. J Hand Surg Am 2009;34:1595-602. https://doi.org/10.1016/j.jhsa.2009.05.017
10. Stoffelen D, De Smet L, Broos P. The importance of the distal radioulnar joint in distal radial fractures. J Hand Surg Br 1998;23:507-11. https://doi.org/10.1016/s0266-7681(98)80134-4
11. Rotella JM, Rotella P. Nueva interpretación de los estabilizadores anatómicos en la fractura de muñeca. Parte II: patrones de lesión de las fracturas de radio. Rev Iberoam Cir Mano 2015;43(1):20-7. https://doi.org/10.1016/j.ricma.2015.06.005
12. Van Leerdam RH, Wijffels MME, Reijnierse M, Stomp W, Krijnen P, Schipper IB. The value of computed tomography in detecting distal radioulnar joint instability after a distal radius fracture. J Hand Surg Br 2017;42(5):501-6. https://doi.org/10.1177/1753193416682682
13. Daneshvar P, Chan R, MacDermid J, Grewal R. The effects of ulnar styloid fractures on patients sustaining distal radius fractures. J Hand Surg Am 2014;39(10):1915-9. https://doi.org/10.1016/j.jhsa.2014.05.032
14. Hauck RM, Skahen J 3rd, Palmer AK. Classification and treatment of ulnar styloid nonunion. J Hand Surg Am 1996;21(3):418-22. https://doi.org/10.1016/S0363-5023(96)80355-8
15. Richards RS, Bennett JD, Roth JH, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am 1997;22:772-6. https://doi.org/10.1016/S0363-5023(97)80068-8
16. Kim JK, Yun YH, Kim DJ, Yun GU. Comparison of united and nonunited fractures of the ulnar styloid following volar-plate fixation of distal radius fractures. Injury 2011 42:371-5. https://doi.org/10.1016/j.injury.2010.09.020
17. Ozaka Y, Iba K, Oki G, Sonoda T, Yamashita T, Wada T. Nonunion of the ulnar styloid associated with distal radius malunion. J Hand Surg Am 2013;38:526-31. https://doi.org/10.1016/j.jhsa.2012.12.006
18. Haugstuedt JR, Berger RA, Nakamura T, Neale P, Berglund L, An KN. Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg Am 2006;31:445-51. https://doi.org/10.1016/j.jhsa.2005.11.008
19. Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults. A descriptive arthroscopic study in 50 patients. J Hand Surg Br 1997;22:638-43. https://doi.org/10.1016/s0266-7681(97)80364-6
20. Oskarsson GV, Aaser P, Hjall A. Do we underestimate the predictive value of the ulnar styloid affection in Colles fractures? Arch Orthop Trauma Surg 1997;116:341-4. https://doi.org/10.1007/bf00433986